Staphylococcus Aureus Mastitis: Cause, Detection, and Control
By G.M. Jones, Professor of Dairy Science and Extension Dairy Scientist, Milk Quality & Milking Management, Virginia Tech; T.L. Bailey, Jr., Assistant Professor, Virginia-Maryland College of Veterinary Medicine, and Extension Veterinarian, Virginia Tech; J. R. Roberson, Assistant Professor, Virginia-Maryland Regional College of Veterinary Medicine, Virginia Tech. Table of Contents
Table of ContentsSummary
Damage Caused by S. aureus Mastitis
Transmission of S. aureus Infections
Detection of S. aureus Mastitis
Control of S. aureus Mastitis
Prevention of New Infections
Conclusions
References
Summary
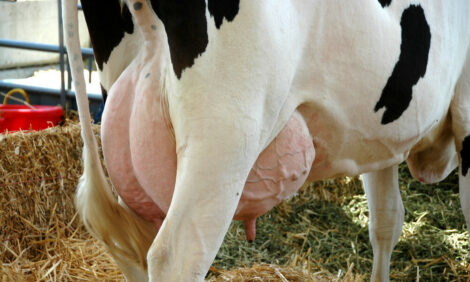
Mastitis caused by Staphylococcus aureus (S. aureus) bacteria is extremely difficult to control by treatment alone. Successful control is gained only through prevention of new infections and cow culling. S. aureus organisms colonize abnormal teat ends or teat lesions. Milkers' hands, wash cloths, teat cup liners, and flies are ways in which the infection can be spread from cow to cow. The organisms probably penetrate the teat canal during milking. Irregular vacuum fluctuations impact milk droplets and bacteria against the teat end with sufficient force to cause teat canal penetration and possible development of new infection. Infected cows must either be culled, segregated from the milking herd and milked last or milked with separate milking units, or teat cup liners must be rinsed and sanitized after milking infected cows.One of the most common types of chronic mastitis is caused by the bacteria, Staphylococcus aureus. Often, it is subclinical, where there is neither abnormal milk nor detectable change in the udder, but somatic cell count has increased. Some cows may flare-up with clinical mastitis, especially after calving. The bacteria persist in mammary glands, teat canals, and teat lesions of infected cows and are considered contagious. The infection is spread at milking time, when S. aureus contaminated milk from infected cows comes into contact with teats of uninfected cows, and the bacteria penetrate the teat canal. Once established, S. aureus usually does not respond to antibiotic treatment, and infected cows eventually must be segregated or culled from the herd. In some herds with somatic cell counts (SCC) below 200,000, dairy managers have not been able to eradicate S. aureus , even when they practiced standard milking time hygiene techniques (Roberson et al., 1994).
Cows infected with S.aureus do not necessarily have high SCC. During 1978-1980, we collected 26,739 aseptic milk samples from cows in 28 herds and found 10% infected with S. aureus (Jones et al., 1984). Only 60% of the infections were found in cows producing milk with more than 200,000 SCC. In several research trials, 3-8% of first lactation cows were found infected with S. aureus at calving. Many remain infected throughout the first lactation and are reservoirs for infecting other cows in the herd. Although as many as half of the cows with high SCC may be infected with S. aureus, somatic cell counts alone are not sensitive enough to positively diagnose S. aureus infections.
Damage Caused by Staphylococcus aureus Mastitis
S. aureus bacteria produce toxins that destroy cell membranes and can directly damage milk producing tissue. White blood cells (leukocytes) are attracted to the area of inflammation where they attempt to fight off the infection. Initially, the bacteria damage the tissues lining the teat and gland cisterns within the quarter. Then they move up into the duct system and establish deep-seated pockets of infection in the milk secreting cells (alveoli). This is followed by walling-off of bacteria by scar tissue and the formation of abscesses, which is responsible for the poor response to antibiotic treatment. Alveolar and duct cells may be destroyed and milk yield is reduced. These degenerated cells may combine with leukocytes and clog the milk ducts that drain the alveolar areas, contributing to further scar tissue formation. The ducts may reopen and release S. aureus organisms to other areas of the mammary gland. Further abscess formation occurs. Eventually, these become quite large and can be detected as lumps within the udder.Clinically infected quarters often show moderate swelling and visible signs of garget or chunks of milk, especially in forestrippings. Acute S. aureus infections generally develop late in the lactation or just prior to calving . However, the clinical symptoms (udder swelling or hardness, changes in appearance of milk) do not show up until calving or early in the next lactation. It becomes difficult to successfully treat an infection because drugs are not able to penetrate to all infection sites and because the bacteria live inside the white blood cells. S. aureus produces an enzyme that inactivates most penicillin-based treatments, resulting in ineffective antibiotics.
Transmission of Staphylococcus aureus Infections
The major reservoirs of these organisms are infected udders, teat canals, and teat lesions, but these bacteria also have been found on teat skin, muzzles, nostrils, and vagina. The bacteria are spread to uninfected quarters by teat cup liners, milkers' hands, wash cloths, and flies. There is some evidence that aerosols play some role in the spread of this organism. Staphylococci do not persist on healthy teat skin but readily colonize teat canals if there are lesions near the teat end. The organisms multiply in infected lesions or colonized teat canals and can readily enter the udder. Infected heifers at calving may represent the most important reservoir to uninfected herdmates. How heifers become infected before calving is unknown at this time. Mastitis control programs need to address the presence of this disease in heifers.Detection of Staphylococcus aureus Mastitis
Culture of bulk tank milk is easy, economical, and is an important aid in determining the microbiological cause of mastitis in the herd. This should be conducted in herds where DHI SCC score is 3.3 or above, or the average actual SCC is above 250,000, or more than 0.5 percent of the cows are withheld from the bulk tank on any day because of clinical mastitis. A culture of only one bulk tank sample is not a complete guarantee that contagious mastitis will be detected as S. aureus infected cows may shed the organism intermittently. Sample three consecutive bulk tanks.Freeze the first two samples. Commingle these two with the third for culturing. Check with your State Lab to see if they will conduct cultures and test for bacteria count, lab pasteurized count, preliminary incubation count, and somatic cell count. A small fee probably will be charged, but it should be worthwhile to test bulk tank samples monthly. Some S. aureus herds have histories of gradually increasing SCC but with very few clinical cases. Use the California Mastitis Test (CMT) on cows with elevated DHI SCC to determine which quarters may be infected. In herds with acute mastitis problems, milk samples from clinical mastitis quarters should be collected aseptically and cultured. Early identification of the infection before the bacteria have an opportunity to invade deep within the udder and form abscesses is important.
Control of Staphylococcus aureus Mastitis
The most effective control is to prevent new infections by minimizing or eliminating conditions that contribute to the exposure of teat ends through spread of infections from cow to cow and conditions which allow bacteria to contaminate and penetrate the teat canal. In addition, certain nutritional components enhance the animal's resistance to mastitis. Supplementation of the diet with vitamin E and selenium, vitamin A and beta-carotene, and balancing dietary copper and zinc content to meet requirements have reduced mastitis.A. Hygienic Procedures
Milkers should wear rubber gloves. Forestrip 5 powerful squirts of milk from each quarter and check for abnormal milk or flakes. Knock dirt off teats. If teats are very dirty, wash them with a sanitizing solution; use low volumes of water; do not use a common cloth or sponge. Pre-dip with a tested disinfectant, applying with a dipper or cup, not spraying, and allow 30 seconds contact time. Use a separate paper or cloth towel to dry teats and scrub teats five times or 20 seconds (Rasmussen et al., 1991). Towels must not be used on more than one cow. Attach milking unit within 1 to 1.5 mins after beginning of pre-milking preparation. Examine teat ends for chaps, cracks, or lesions that harbor mastitis-causing bacteria. Use an effective post-milking teat dip and cover most of each teat (at least the bottom 1/2 to 2/3). Discard teat dip left in dip cup at end of each milking, rinse cups with water after every milking and dry.
B. Milk First Lactation Cows First if Possible
Uninfected first lactation cows should be milked before older cows carrying subclinical mastitis infections, if possible. If the milking herd can be grouped, a separate group for uninfected first lactation cows is recommended, which can be milked first and fed differently. Since heifers may be infected at calving, aseptic milk samples should be collected shortly after calving and frozen. These samples could be cultured if the cow's DHI SCC score exceeds 4 or clinical mastitis develops. If first lactation cows cannot be separated from infected or high SCC cows, problem cows with clinical mastitis and those receiving antibiotic therapy must be milked last, or milking units must be disinfected with sanitizer after milking infected cows.
C. Milk S. aureus Infected Cows Separately or Last Cows with clinical mastitis, S. aureus infections or those that have been treated with antibiotics should be milked last, or milked with separate milkers or milking units equipped with backflush to avoid spread of infection via contaminated teat cup liners. Segregation of S. aureus infected cows has been proven to significantly reduce the prevalence of S. aureus mastitis and bulk tank somatic cell counts (Wilson et al., 1995).
D. Milking Equipment
S. aureus infections probably occur during milking when organisms penetrate the teat canal. Irregular vacuum fluctuations, caused by liner slips, flooded lines, etc., may cause a backflow of milk against the teat end with sufficient force to impact any bacteria (from contaminated liners, dirty or wet teats, everted teat ends) deeply into the teat canal and into the teat cistern. Lesions and damage to the teat provide sites for the bacteria to become established and prevent them from being flushed out of the teat.
Try to minimize conditions that are associated with high impact force against the teat end, including liner slips, excessive temporary vacuum losses, low vacuum reserve, inefficient vacuum regulation, and abrupt milking unit removal. Do not remove teatcups from the cow until the vacuum has been shut off. Research has shown that slipping teat cup liners may cause 10-15% of new mastitis infections. Slipping early in milking often results from low vacuum level, blocked air vents, or restrictions in the short milk tube. Slipping in late milking is commonly caused by poor cluster alignment, uneven weight distribution in the cluster, or poor liner condition. Incomplete milking can be caused by poor type or condition of liner, mismatch between claw inlet and short milk tube, clusters too light, clusters that do not hang evenly under the udder, or high milking vacuum levels (Halleron, 1997).
Regular preventive maintenance is essential. Vacuum controllers (regulators), pulsators, and air filters need to be cleaned monthly. Rubber that is cracked, flattened, or otherwise deteriorated should be replaced. Teat cup liners, or short pulsator or milk tubes, should be replaced whenever holes are found in them. The milking system should be evaluated every three months or 500 hours of operation, including the following tests: vacuum reserve, vacuum level, vacuum recovery time, vacuum regulator response, pulsator graphs, and stray voltage.
E. Antibiotic Treatment of S. aureus Cows
Treatment will not control this disease but it may shorten the duration of the infection. Treatment effectiveness decreases as cows become older. Cures were only 34% when 89 cows in 10 Dutch herds were treated for subclinical S. aureus mastitis (Sol et al., 1997). The results showed that probability of cure would be low in older cows with high SCC, infected in hind quarters during early and midlactation. S. aureus infections were found in 36% of clinical mastitis cases in Finish herds (Pyorala and Pyorala, 1997). Of these, only 39% responded to treatment. A SCC < one million was 85% accurate in predicting bacteriological cures. Detect and act on developing mastitis problems early. Successful treatment during lactation is greater if detected and treated early and response is lower when treating chronic infections. Cows whose DHI SCC increases to a score of 5 or actual SCC above 300,000 should be checked with the California Mastitis Test to determine which quarters may be infected. Milk samples from positive quarters should be cultured. Use a strip cup or similar device for detecting abnormal milk. New clinical infections should be treated promptly and appropriately, especially in first lactation cows. Tissue damage can be minimized if treated during early stages of infection. Consult your veterinarian regarding intramammary or other treatments. Use the DHI SCC or CMT to monitor whether treated cows remain low or if infection recurs and becomes chronic.
If a new S. aureus infection is not treated, the bacteria penetrate the mammary gland tissues and the cow attempts to wall off the area, forming an abscess and eventual scar tissue (Belschner et al., 1996). These areas of scar tissue are difficult to penetrate with drugs in effective concentrations. The bacteria also escape the killing effects of some antibiotics in the neutrophils (white blood cells). As these white blood cells attempt to remove bacteria through phagocytosis, many organisms become inactive and are not killed by the neutrophil or by antibiotics which penetrate the cell. The bacteria may remain inactive inside the neutrophil. When the cells die, usually 5-7 days, the bacteria are released to resume cell division and the infection process. The development of antibiotic resistance and formation of L-forms during treatment with some beta-lactam antibiotics (e.g., penicillin) are additional reasons for therapy failures. Chronic S. aureus cows usually have high SCC, abnormal mammary tissue, and recurrent cases of clinical mastitis.
To give an example of the futility of treatment during lactation, pirlimycin is one of the most effective compounds that Pharmacia and Upjohn Co. has found against S. aureus. Its chemical nature allows it to penetrate mammary tissues extremely well. In mastitis data presented to FDA, two tubes were administered 24 hours apart and the cure rate was 36.6%; only 1.1% of non-treated controls recovered spontaneously. The cow cure rate was 49.4% for treatment in field cases. But trials at Louisiana State University and Iowa State University with chronically infected S.aureus cows found cure rates of 12% or less. An extra label treatment duration was experimented with to provide effective drug levels beyond the expected life of the neutrophil. Single quarter extended treatment with repeated label doses of Pirlimycin may not provide adequate drug concentrations for a long enough period of time to effect a bacteriologoical cure on chronically infected animals. Four quarter extended treatment with repeated label doses will provide adequate therapeutic concentrations for many S. aureus bacteria. A cure rate of 50% at 4 weeks after treatment was found in more than 100 treated cows. Whether these cure rates justify the additional expenses and effort (Belschner et al., 1996), not to mention the potential risk of extra label use and antibiotic residue, is unknown.
F. Dry Cow Therapy
Administration of specially formulated dry cow treatments will help prevent new S. aureus infections during the dry period and also will eliminate many existing infections present at drying off. Dry treatment is more effective in eliminating infections than lactating treatment. During the first 2 weeks and the last 7-10 days of the dry period, cows are very susceptible to becoming infected. When cows are not dry treated, spontaneous cures have been very low. Dry cow antibiotic treatment is very cost effective (Kirk et al., 1997). When a cow is dried-off, treat all quarters with a commercial dry cow product. To dry off, cows must be milked out completely, teats dipped in post-milking teat dip and blotted dry after 30 seconds contact time. Scrub teats with alcohol pads before partially inserting tube into teat (one-eighth inch). Teat dip again after treatment. Turn cows into clean, dry environment.
G. Pregnant Heifers
New infections can be found in many heifers, either at calving or in early lactation. As many as one-third of these infections may be caused by S. aureus. Often these S. aureus infections, if untreated, become clinical and recur throughout the first lactation and into the second lactation. Several newly tested procedures can be used on heifers before they calve. Pregnant heifers should not be grouped with dry cows.
Dry Cow Therapy- Louisiana studies have examined the feasibility of giving antibiotic therapy to heifers (Nickerson et al., 1995). A dry cow product containing penicillin and dihydrostreptomycin was administered at the first, second, or third trimester of pregnancy in 35 bred heifers from four herds. Although prevalence of infection and SCC was reduced by treatment in all three groups of heifers, heifers dry-treated during the second trimester of pregnancy demonstrated greater reduction in mastitis and SCC at calving. It is recommended that heifers can be treated with dry cow treatment at 60 days before expected calving date. Properly clean and disinfect teat ends before and after treatment. Check milk for presence of antibiotic residue at 3 to 5 days after calving and before milk is put into milk tank.
Lactating Cow Therapy- In Tennessee, a lactating cow antibiotic treatment containing either cloxacillin or cephapirin was administered to heifers at 7 to 10 days before expected calving (Oliver et al., 1992). Mastitis infections were reduced. Cephapirin gave better treatment results but also resulted in some antibiotic residue in milk at 3 days after calving. The residue was not present when heifers were treated at 14 days before expected calving. It can be recommended that heifers can be treated with lactating cow mastitis treatment at 14 days before expected calving. Use precautions indicated under Dry Cow Therapy.
Milk Heifers Before Calving- Start heifers through milking parlor 2-4 weeks before expected calving (Wilson, 1997). Do not save milk. Calves born to these heifers will need fresh or frozen colostrum from older cows.
H. Precautions at Calving
Many mastitis infections occur at the time of calving or the preceding 1-2 weeks. A well-drained pasture is preferred as a calving area, with no access to ponds, swampy area, or drainage ditches. A clover-grass sod is desired, in contrast to fescue or muddy, "beaten-up" lots. Lots and pastures should be managed to prevent muddy areas where cattle would lie down. Filthy, damp, or muddy pens, lots, or pastures continually expose the teat end to a barrage of bacteria. Pens should be well bedded, clean, dry, and comfortable. Selenium-vitamin E supplementation or injections at 2-3 weeks before expected calving have been shown to reduce mastitis after calving. However, vitamin E levels of at least 1,000 IU/day during the dry period and 500 IU/d during lactation were more beneficial than National Research Council's recommended 100 IU/d (Weiss et al., 1997). Other minerals and vitamins shown to reduce incidence of mastitis include vitamin A/beta-carotene, copper, and zinc.
Prevention of New Staphylococcus aureus Infections
S. aureus infected cows must be isolated from other cows to prevent spread of infection. This may be the most important preventative practice. Infected cows should be marked with unique, visible identification, such as special colored leg bands or neck chains. Possible means of isolation include:- Do not milk cows and heifers with the same teatcup/claw unit used to milk mastitis-problem cows.
- Segregate S. aureus infected cows into one group and milk last. Another alternative is to sort-out infected cows before each milking and restrain them in an isolation pen until all other cows have been milked. In a short period of time, these cows will become trained to sort.
- If heifers or cows are purchased, they should be segregated until milk samples can be cultured and their mastitis pathogen status can be determined. If possible, examine DHI SCC of cows before agreeing to purchase them.
- Automatic backflush units will rinse both liners and claw with water and disinfect with sanitizer.
- Manually backflush and/or sanitize teatcup liners after milking infected cows using iodine (25 ppm) or chlorine (100 ppm, or 3 tbs/5 gal water) solutions. Hang to dry for short periods of time.
- Cull infected cows, especially those with other problems. Often, it is not economically feasible to cull a staph cow that produces 80-90 lb milk. However, any cow that has had clinical mastitis in the same quarter for three or more occasions, or any cow whose milk has been withheld from shipment for more than 28 days during the current lactation, should be considered for culling from the herd. It is important to keep mastitis records, including cows and quarters treated and treatment used.
- Place S. aureus infected cows on a do-not-breed list. Cull them when their milk is no longer needed (e.g., to make base) or they have been in milk 305 days.
- Biting flies traumatize the teat end. Flies also carry a number of mastitis-causing organisms that can colonize these teat lesions. Elimination of fly breeding sites is one aspect of fly control. Flies breed in decaying feed or manure that has accumulated, including exercise yards, calf pens, and box stalls. Other options include backrubbers, feed additives and ear or tail tags. In one trial where tail tags contained insecticide, only 1 of 100 heifers had a mastitis infection compared to 18 of 100 untagged heifers.
- It is unclear whether waste milk from S. aureus-infected cows is a problem. There is no research evidence that it is, as long as calves cannot suckle others. However, high fly infestation has been related to teat lesions and S. aureus infections. There is the possibility that flies could transmit S. aureus infections from waste milk to teat ends.
Conclusions
Dairy managers who are more aware of their herd's status relative to mastitis have herds with lower SCC (Hutton et al., 1990). They tend to be better informed. They attend more dairy informational meetings, short courses, and DHI meetings. They read dairy magazines. They are more likely to use a computer to assist them in management. They have higher production per cow with fewer intramammary infections, especially S. Aureus, but also environmental streptococci. They more frequently milk clinical cows last and higher producing cows first, using rubber gloves. They wash udders with disinfectant, apply teat dip, and disinfect milking units between cows. They disinfect teat ends prior to as well as after intramammary therapy. Infusion tubes are only partially inserted. They use automatic takeoffs and their milking systems have greater vacuum reserve. Bedding for maternity and milking cows is drier and there is no standing water in pastures. They cull cows because of mastitis.References
Belschner, A.P., J.W. Hallberg, S.C. Nickerson, and W.E. Owens. 1996. Staphylococcus aureus mastitis therapy revisited. p. 116-122 in Proc. 35th Annu. Mtng., Nat'l Mastitis Counc., Madison, WI.
Halleron, R. 1997. Liner slips cause 10 to 15 percent of new infections. p. 624 in Aug. 25 issue of Hoard¼s Dairyman.
Hutton, C. T., L. K. Fox, and D. D. Hancock. 1990. Mastitis control practices: Differences between herds with high and low milk somatic cell counts. J. Dairy Sci. 73:1135.
Jones, G.M., R.E. Pearson, G.A. Clabaugh, and C.W. Heald. 1984. Relationships between somatic cell counts and milk production. J. Dairy Sci. 67:1823.
Kirk, J.H., S.L. Berry, I.A. Gardner, J. Maas, and A. Ahmadi. 1997. Dry cow antibiotic treatment in a herd with low contagious mastitis prevalence. Proc. 36th Annu. Mtng., Nat'l Mastitis Coun., p. 164., Madison, WI.
Nickerson, S. C., W. E. Owens, and R. L. Boddie. 1995. Mastitis in dairy heifers: Initial studies on prevalence and control. J. Dairy Sci. 78:1607.
Oliver, S. P., M. J. Lewis, B. E. Gillespie, and H. H. Dowlen. 1992. Influence of prepartum antibiotic therapy on intramammary infections in primigravid heifers during early lactation. J. Dairy Sci. 75:406-414.
Pyorala, S. and E. Pyorala. 1997. Accuracy of methods using somatic cell count and N-acetyl-B-D-glucosaminidase activity in milk to assess the bacteriological cure of bovine clinical mastitis. J. Dairy Sci. 80:2820-2825.
Rasmussen, M.D., E.S. Frimer, D.M. Galton, and L.G. Petersson. 1992. The influence of premilking teat preparation and attachment delay on milk yield and milking performance. J. Dairy Sci. 75:2131.
Roberson, J.R., L.K.Fox, D.D.Hancock, J.M.Gay and T.E. Besser. 1994. Ecology of Staphylococcus aureus isolated from various sites on dairy farms. J. Dairy Sci. 77:3354.
Sol, J., O. C. Sampimon, J. J. Snoep, and Y. H. Schukken. 1997. Factors associated with bacteriological cure during lactation after therapy for subclinical mastitis caused by Staphylococcus aureus. J. Dairy Sci. 80:2803-2808.
Weiss, W. P., J. S. Hogan, D. A. Todhunter, and K. L. Smith. 1997. Effect of vitamin E supplementation in diets with a low concentration of selenium on mammary gland health of dairy cows. J. Dairy Sci. 80:1728-1737.
Wilson, D.A., R.N.Gonzalez and P.M.Sears. 1995. Segregation or use of separate milking units for cows infected with Staphylococcus aureus: Effects on prevalence of infection and bulk tank somatic cell count. J. Dairy Sci. 78:2083.
Wilson, K.O. 1997. Streamlined dairy premilks its heifers prior to calving. p. 348 in April 25 issue of Hoard¼s Dairyman.
March 1998